What is Centers for Medicare & Medicaid Services (CMS)?
The Centers for Medicare and Medicaid Services (CMS) is a federal agency within the U.S. Department of Health and Human Services (HHS). CMS administers major healthcare programs that provide health coverage to more than 160 million Americans. These programs include Medicare, Medicaid, the Children's Health Insurance Program (CHIP) and coverage provided through the Health Insurance Marketplace.
CMS also plays a central role in shaping national health policy and overseeing initiatives that promote the adoption of health information technology (health IT), such as electronic health records (EHRs), data interoperability and value-based reimbursement models.

History of Centers for Medicare and Medicaid Services
CMS has evolved significantly since its origins:
- 1965. Medicare and Medicaid were established under the Social Security Administration.
- 1977. The Health Care Financing Administration (HCFA) was created to manage federal healthcare programs.
- 2001. HCFA was renamed the Centers for Medicare & Medicaid Services to reflect its mission and scope better.
Today, CMS manages a significant portion of federal healthcare spending and is instrumental in shaping coverage, quality, reimbursement and innovation policy.
CMS reimbursement and regulatory functions
CMS is responsible for implementing several key healthcare programs and reimbursement systems in the U.S., including the following:
- Medicare. The federal health insurance program for individuals aged 65 and older and some younger individuals with disabilities.
- Medicaid. A state-administered, needs-based program providing healthcare coverage to low-income individuals and families.
- CHIP. Provides health coverage to eligible children in families with incomes too high to qualify for Medicaid but too low to afford private coverage.
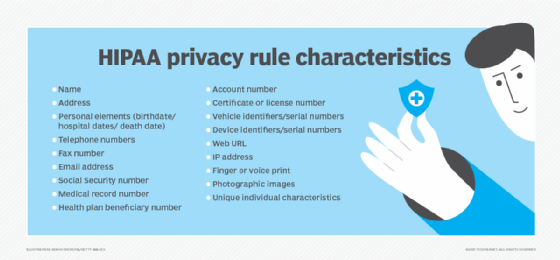
- Health Insurance Portability and Accountability Act (HIPAA). Although primarily enforced by the HHS Office for Civil Rights, CMS oversees certain HIPAA administrative simplification provisions.
- Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA is a key legislative reform that replaced the Sustainable Growth Rate formula with value-based payment systems.
Merit-based and value-based reimbursement
CMS administers several programs under MACRA that shift reimbursement from fee-for-service to value-based healthcare models:
- Merit-Based Incentive Payment System (MIPS). Adjusts Medicare reimbursement rates based on performance across four categories: quality, cost, improvement activities and promoting interoperability.
- Alternative Payment Models. Offer additional incentives for clinicians to provide high-quality, cost-efficient care through mechanisms like bundled payments and accountable care organizations (ACOs).
These initiatives aim to improve patient outcomes, increase care coordination and reduce healthcare costs.
CMS and health IT programs
CMS has played a pivotal role in advancing health information technology in the U.S. Following the 2009 passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act, CMS launched the Medicare and Medicaid EHR Incentive Programs, known as Meaningful Use.
Under this program, eligible professionals and hospitals received financial incentives for adopting, implementing and meaningfully using certified EHR technology. The program ran in multiple stages and helped catalyze widespread EHR adoption nationwide.
In 2017, the Meaningful Use program was restructured into the Promoting Interoperability program, which is now part of MIPS. CMS continues to evaluate whether providers are using certified health IT in a manner that improves patient care and data exchange.
Collaboration with ASTP/ONC
CMS works closely with the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health Information Technology (ASTP/ONC), which has several key responsibilities:
- Certifying health IT systems used in CMS programs.
- Defining interoperability standards and measures.
- Updating data exchange, privacy and security requirements.
While ASTP/ONC defines technical criteria for EHRs and interoperability, CMS enforces how these systems are used to meet clinical and regulatory goals. As of 2023, nearly all hospitals and most physician practices in the U.S. use certified EHRs. CMS continues to play a leading role in health IT policy development and oversight.
CMS and the Health Insurance Marketplace
CMS oversees the Health Insurance Marketplace, also known as the Exchange, which was established under the Affordable Care Act. The Marketplace allows individuals and small businesses to shop for and enroll in qualified health plans.
CMS has several responsibilities related to the Exchange:
- Operating the federal Marketplace at HealthCare.gov.
- Partnering with state-based Marketplaces.
- Enforcing coverage standards and eligibility criteria.
- Managing premium tax credits and subsidies.
Each year, CMS leads open enrollment and works to improve consumer access to affordable insurance coverage.
CMS innovation and the CMS Innovation Center
The Center for Medicare & Medicaid Innovation (CMMI), a division within CMS, was created under the Affordable Care Act to test and implement innovative payment and service delivery models.
CMMI has spearheaded the following initiatives:
- Comprehensive Primary Care Plus
- Next Generation ACO Model
- Kidney Care Choices Model
- Global and Professional Direct Contracting
These programs aim to reduce costs while improving care quality, access and outcomes for Medicare and Medicaid beneficiaries. CMMI also supports advanced models that address health equity, social determinants of health and care integration.
Balancing AI deployments with HIPAA compliance poses risks. Learn how to navigate major compliance risks associated with AI and HIPAA.




