What is HL7 (Health Level Seven International)?
HL7 (Health Level Seven International) is an accredited, not-for-profit organization that develops frameworks and standards used worldwide for health IT applications to retrieve, exchange, share and integrate electronic health information.
HL7 standards define formats for structuring and exchanging healthcare data so that different clinical and administrative systems, such as electronic health record (EHR) software and billing applications, can share information quickly and efficiently. Through common language, structure and data types, these standards are designed to facilitate interoperability between disparate healthcare technology systems.
Important HL7 standards
There are six main categories of HL7 standards:
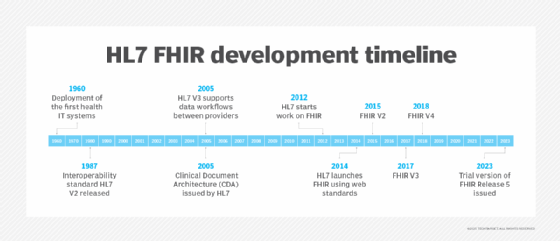
- HL7 Version 2.x (HL7-v2.x). HL7-v2 is the most widely used messaging standard and format for electronic data exchange among heterogeneous IT systems/interfaces in healthcare environments. It was first developed in 1987 as HL-v2 and achieved widespread use by the mid-1990s. HL7 developed many versions of HL-v2, including v2.2, v2.3.1, v2.4, all the way to v2.9.
- HL7 Version 3 (HL7-v3). HL7-v2 contained several semantic inconsistencies. An attempt to eliminate these inconsistencies by HL7 International led to the development of HL7-v3. This standard included a well-defined data model called RIM (Reference Information Model) to represent clinical data in a standard format. HL7-v3 also introduced the CDA standard to simplify the creation of patient discharge summaries. However, to use its data exchange tools, application users need to understand RIM, which can be challenging for some healthcare organizations.
- Clinical Document Architecture (CDA). CDA is an ISO-approved document-markup standard to describe clinical documents, such as discharge summaries and progress notes, for the purpose of health information exchange. CDA specifies the structure and semantics of clinical documents to facilitate such exchanges between healthcare providers. CDA is part of the HL7 v3 standard and is based on XML (meaning CDA documents are XML-encoded templates).
- Consolidated CDA (C-CDA). C-CDA is used in ONC meaningful use-certified EHRs to consolidate nine previous CDA templates into one document, thus facilitating easier exchange of CDA documents. C-CDA documents (also represented in XML like CDA documents) can include both structured information, like medication lists, and unstructured information, like medical images.
- Continuity of Care Document (CCD). A standard jointly developed by HL7 International and AST, CCD is designed to help healthcare providers share patient Continuity of Care (CCR) summary data. CCD provides templates to represent the various sections of a summary record, with the patient data encoded using XML. The templates are expressed as constraints on CDA. CCDs are human-readable and can be displayed on any standard web browser.
- Fast Health Interoperability Resources (FHIR). This interoperability standard facilitates the exchange of healthcare information, such as clinical and administrative data, between healthcare organizations, regardless of how they store the information in their systems. FHIR has two main components: resources and APIs. Resources are modular components that form categories of healthcare data (such as patients or laboratory results), while the APIs use RESTful interfaces for interoperable exchange of the resources.
Benefits of HL7 standards
The HL7 standards are accepted and used throughout the world (in fact, they are the de facto standards for information exchange in healthcare IT) because they simplify the sharing of healthcare data between health IT applications. Also, the standards support clinical practice, as well as the delivery, management and evaluation of health services. This can then help healthcare providers to make better use of available data in order to deliver better care to patients.
The HL7 standards are meant to standardize data interchanges between systems, not the systems themselves. Also, the number of required data fields in the abstract messages are deliberately kept to a minimum. These fields are needed to support the logic of the relationships among the messages. Many other specified fields are optional. Such flexibility allows different institutions to apply the standards in different ways. The specifications also allow healthcare organizations to add messages or portions of messages that are unique to them. At the same time, standard conventions are provided to prevent conflict with future versions of the standards.
HL7 also promotes global interoperability in healthcare IT by providing guidance about how to implement its standards. It also provides error communication guidelines, incorporating XML compatibility to simplify the encoding of clinical data for transmission, storage and display in healthcare IT systems.
The HL7 standards are mainly concerned with electronic data exchange in healthcare environments. However, HL7 also supports several other standards for these environments:
- Imaging standards like DICOM (Digital Imaging and Communications in Medicine).
- Electronic Data Interchange standards like ASC X12.
- Laboratory data reporting standards like ASTM 1238-88.
- IEEE P1157 standards for Medical Data Interchange.
History of HL7 International and HL7 standards
HL7 International was founded in 1987 and accredited by the American National Standards Institute (ANSI) in 1994. Its primary mission is to develop universal and common standards, technologies and frameworks that facilitate the seamless interoperability of healthcare data and healthcare IT systems.
The organization has more than 1,600 members from over 50 countries. Members include healthcare providers, payers, pharmaceutical companies, researchers and consulting firms, as well as government stakeholders, policy groups and healthcare vendors/suppliers that jointly participate in the creation and maintenance of standards for healthcare information exchange.
In addition to its primary standards, HL7 has developed RIM, a static reference ISO model of health and healthcare information. RIM can be used to develop further health informatics specifications.
Thousands of volunteers worldwide work together to define, develop and maintain HL7 standards. These volunteers are usually grouped into "work groups," such as Clinical Decision Support, Clinical Genomics, Vocabulary or Patient Administration. Most work groups own a specific conceptual subdomain, although some work across multiple conceptual domains.
HL7 develops new standards using formal bylaws and a consensus-based balloting system modeled on the balloting systems of other relevant healthcare data messaging standards organizations. In addition, the bylaws and balloting procedures conform to ANSI's requirements. Per the HL7 balloting system, work groups must gather and reconcile feedback on a new specification and follow a formal decision-making process before publishing the spec as a normative standard.
HL7 and OSI model
The "7" in HL7 refers to Layer 7 of the ISO Open Systems Interconnection (OSI) reference model. The OSI model is a seven-layered conceptual model that describes how different systems communicate with each other using common standards and protocols.
The seventh layer of the OSI model is the application layer. This layer interfaces directly to application processes and includes functions like data synchronization between computer systems. The HL7 standards sit in the application layer because they provide a common language for health IT applications to "talk" to each other. In doing so, the standards help the applications store, share and move data easily and efficiently. This can then help healthcare providers to make better use of the available data to guide their clinical decisions, evaluate their health services and deliver higher-quality care to patients.
Explore how HL7 FHIR APIs offer significant opportunities across various areas, including clinical care, research, health information exchange and public health, highlighting their potential to drive innovation in the healthcare sector.