What is meaningful use stage 3?
Meaningful use stage 3 is the third phase of the Medicare and Medicaid Electronic Health Record (EHR) Incentive Program, commonly called the "meaningful use" (MU) program. The Centers for Medicare and Medicaid Services (CMS) established Stage 1 in 2011; Stage 3 emerged in 2016.
Each stage of the MU program sets specific objectives. To qualify for incentive payments, eligible professionals (EPs), hospitals and critical access hospitals (CAHs) in the U.S. needed to achieve the objectives. The goal was to encourage medical providers to adopt, implement, upgrade and demonstrate meaningful use of certified EHR technology (CEHRT) using specific metrics and performance measures. MU stage 3 was intended to get eligible medical providers to properly capture electronic data, use it and demonstrate meaningful use to improve patient outcomes. Meeting the objectives of all three stages would make EPs and CAHs eligible for full reimbursement from Medicare (the largest healthcare payer in the U.S.).
Meaningful use stages 1, 2, 3
Stage 1 emphasized the proper capture and sharing of electronic data using EHR technology. It included nine core objectives and one public health objective. EPs, eligible hospitals and CAHs could receive their incentive payment if they meet all these objectives.
Stage 2, which began in 2014, required medical providers to advance their clinical processes and EHR capabilities to a wider portion of their patient populations. It included new objectives and measures and higher thresholds than Stage 1. It also simplified the MU program by eliminating certain measures the CMS deemed irrelevant to report, such as patient demographics, smoking status or patient clinical summaries for each office visit.
EPs that first attested in 2014 or 2015 could not attest to Stage 1 post-2015 (because Stage 1 was eliminated). Instead, they had to attest to the new, Modified Stage 2. With nine core objectives and one public health objective, Stage 2 was provided several alternative measures and exclusions so it looked similar to Stage 1.
Stage 3 built on the earlier stages and tried to drive interoperability between EHRs, and, ultimately, help medical providers provide better care to patients and improve outcomes. Several quantifiable and clear measures were included to help EPs meet the objectives. Thresholds for some measures were increased but providers gained more flexibility regarding the use of CEHRT versions.
MU stage 3 and reporting periods
EPs could begin Stage 3 in 2017 or, optionally, wait until 2018. For 2017, EPs could choose to attest to either Modified Stage 2 or Stage 3 of the program.
If they chose to continue to attest to Stage 2, a reporting period of a full calendar year applied. For Stage 2 attestation, they could use a 2014 edition CEHRT.
EPs choosing to attest to Stage 3 had a 90-day reporting period; this applied to EPs attesting for the first time in 2017, regardless of whether they chose to attest to Stage 2 or Stage 3.
For 2018, all EPs were required to attest to Stage 3. For successful Stage 3 attestation in 2018, EPs had to use a 2015 edition CEHRT. The reporting period for 2018 was a full year. EPs were also required to meet certain MU objectives, each with its own specific measures.
Meaningful use program requirements
Stage 3 includes all requirements physicians and other providers must meet to receive their Medicare reimbursements and avoid penalties. Between 2011 and 2014, EPs only had to adopt EHRs to qualify for incentive payments. However, from 2015 onward, the program introduced financial penalties for EPs who failed to demonstrate meaningful use of an EHR system.
In Stage 3, physicians and other EPs were required to meet eight overall objectives that covered these areas:
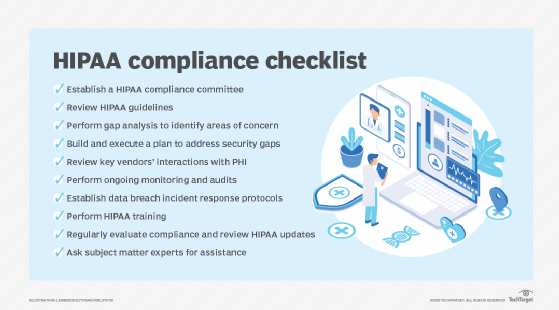
- Protect patients' electronic health information (ePHI) . Eligible physicians and hospitals were required to implement appropriate safeguards (technical, administrative and physical) to protect ePHI. These safeguards could include the following:
- Conducting a Health Insurance Portability and Accountability Act (HIPAA)-compliant security risk analysis (SRA) to assess ePHI vulnerabilities that could lead to data breaches.
- Implementing security updates as necessary.
- Securing ePHI with encryption and other necessary security measures.
- Ensuring that data is stored securely and in encrypted format.
- Correcting identified security gaps or vulnerabilities as part of the risk management process.
- Electronic prescribing (eRx). EPs must generate and transmit at least 60% of their permissible prescriptions electronically using CEHRT.
- Clinical decision support (CDS). EPs were mandated to implement five CDS interventions related to four or more clinical quality measures (CQMs) to improve patients' high-priority health conditions. They were required to enable functionality for drug-drug and drug-allergy interaction checks during the EHR reporting period.
- Computerized provider order entry (CPOE). Under this objective, EPs were required to meet three measures for the recording of medication orders, laboratory orders and diagnostic imaging orders. For each, the threshold was 60%, meaning they had to record at least 60% of each type of order using CPOE.
- Patient electronic access to PHI. To help encourage patient engagement, meaningful use stage 3 includes an objective in which EPs must provide more than 80% of patients access to their own EHRs through a patient portal or some other electronic application of the patient's choice. The application must be configured to meet the technical specifications of the API in the provider's CEHRT. EPs also had to ensure that 80% of patients could download and transmit their health information to a third party of their choice. In addition, EPs had to send educational resources (patient-specific) to more than 35% of their patients.
- Coordination of care through patient engagement. This objective concerned the use of CEHRT to engage with patients (or their authorized representatives) regarding the patient's care. It included three quantifiable measures: 1) more than 10% of patients must view, download or transmit (to a third party) their PHI, 2) more than 25% of all patients must send a secure message electronically and 3) incorporate patient-generated data or data from a nonclinical setting into the EHRs of more than 5% of all unique patients the EP saw during the reporting period.
- Health information exchange (HIE). MU stage 3 made EPs and CAHs responsible for exchanging health information through an HIE with other EPs and CAHs when transitioning or referring a patient out and when receiving a receipt of a patient transition or referral. The measures encourage interoperability in three ways: 1) create a summary of care and electronically transmit more than 50% of patient care transition and referrals using CEHRT, 2) receive or retrieve and incorporate an electronic summary of the care document into the patient record for more than 40% of transitions or referrals received for new patients and 3) perform clinical information reconciliation for more than 80% of transitions or referrals received for new patients.
- Public health and clinical data registry reporting. EPs and CAHs were expected to actively engage with public health by submitting electronic public health data from their CEHRT. They could choose to submit three out of five allowed data types: 1) immunization data, 2) syndromic surveillance data, 3) case reports of reportable conditions, 4) cancer data or health surveys and 5) clinical data.
HIPAA also mandates several practices, such as risk analysis and security audits. Because EPs must comply with HIPAA, the requirements attached to MU objectives make it a must-have to receive incentives.
Deactivation of the meaningful use program and stage 3
In April 2018, the CMS renamed the MU program to the Medicare and Medicaid Promoting Interoperability (PI) Programs for eligible hospitals and CAHs. With the introduction of the Medicare Access and CHIP Reauthorization Act (MACRA), the MU program became one of the four components of the Merit-based Incentive Payment System (MIPS).
MACRA is federal legislation enacted on April 16, 2015, that establishes ways to pay physicians for caring for Medicare beneficiaries; it includes funding for technical assistance for providers and related measure development and sets data sharing requirements.
MIPS consolidates multiple CMS quality programs, including MU and the value-based payment modifier program, into a single program. It includes the Physician Quality Reporting System. Today, MIPs is part of MACRA.
One of the four components or "performance categories" of MIPS is called Advancing Care Information (ACI). ACI replaced the now-sunset MU program in 2017 and accounts for 25% of eligible clinicians' total MIPS composite score. While ACI addresses many of the same reporting objectives and measures as MU stage 3, it gives EPs more flexibility than MU in terms of the following:
- Lowering the number of measures to meet.
- Increasing flexibility on which objectives they could choose to emphasize in their scoring.
- Aligning their reporting with their practice and experience instead of being forced to attain fixed reporting thresholds.
- Focusing more on EHR interoperability and patient engagement rather than processes.
- Eliminating CDS and CPOE objectives.
- Accommodating multiple options for physicians to receive incentives.
- Including a hardship exception for the ACI category for certain physicians who do not use certified EHR technology, so the ACI category score will not lower their MIPS Composite Score to zero and prompt reimbursement obstacles.
With the arrival of MACRA and MIPS, the scoring system of MIPS considers whether EPs are using certified EHR technology and attaining MU, so MU is not obsolete. Healthcare providers continue to use the term to guide their activities regarding the storage of digital information, safeguarding patient information, and the interoperability and exchange of healthcare data.
Achieving nationwide health data interoperability requires streamlining health information exchange participation and adopting standardized data protocols. Learn about the top challenges to widespread health data interoperability.







