What is FHIR (Fast Healthcare Interoperability Resources)?
Fast Healthcare Interoperability Resources (FHIR) is an interoperability standard developed by Health Level Seven International (HL7) to facilitate the exchange of healthcare information between various entities involved in the healthcare ecosystem. These entities can be healthcare providers, patients, caregivers, payers or researchers. The standard allows different computer systems belonging to these various entities to exchange healthcare information, regardless of how each system stores the information.
Accredited by the American National Standards Institute (ANSI), HL7 is a not-for-profit organization that develops and provides frameworks and standards for the sharing, integration and retrieval of clinical health data and other electronic health information.
Importance of FHIR
Electronic health records (EHRs) include a lot of patient information that healthcare providers can access in order to coordinate care and improve care quality. However, EHRs often represent different kinds of patient data in different ways. Also, EHRs and health IT systems continue to be plagued by interoperability problems, which can negatively affect care coordination, generate errors and decrease operational efficiency.
FHIR emerged in 2014 as a draft standard for trial use to address these issues. The aim was to enable health IT developers to build applications for EHRs more quickly and easily, and to enable applications to exchange and retrieve data faster and more easily. In doing so, FHIR facilitated a standardized representation and exchange of information between clinicians and healthcare organizations, regardless of how local EHRs represented or stored the data.
FHIR combines many of the best features of other standards to provide a common, easily adoptable specification for healthcare information interchange. It is also flexible so it can meet the needs of a variety of healthcare use cases. Moreover, it uses widely accepted web technologies to simplify and accelerate its adoption in healthcare settings.
FHIR benefits
As patient healthcare records become increasingly digitized, care providers need a simple way to discover, access and understand the records. They also need the data to be well structured and standardized to make it readable and actionable. FHIR meets all these objectives.
The standard facilitates easy and secure access to healthcare data, including clinical and administrative data, by anyone who is authorized to access the data. These entities might be care providers, such as doctors, or even the patients themselves.
For doctors, FHIR allows them to access the data and use it to inform their patient treatment plans or to coordinate care with other providers.
FHIR can be used as a standalone data exchange standard, or it can also be used with other widely used standards and initiatives that promote their coordinated implementation, such as the following:
- HL7 v2.
- HL7 v3.
- Clinical Document Architecture (CDA).
- Substitutable Medical Applications and Reusable Technologies (SMART) on FHIR.
- Integrating the Healthcare Enterprise.
Interoperability between FHIR and other standards enables healthcare organizations to access data in a standardized way without having to overhaul their existing infrastructure.
Another advantage of FHIR is that it leverages existing and well-known logical and theoretical data models. In doing so, it simplifies implementation and provides a robust yet simple and efficient mechanism for healthcare applications to exchange data. These models also ensure information integrity.
FHIR aligns with HL7's previously defined patterns and best practices and includes mechanisms to ensure traceability to important content models, including the HL7 RIM (Reference Information Model). These alignments and mechanisms remove the need for implementers to have intimate knowledge of the HL7 RIM or HL7 v3, further simplifying FHIR implementation and adoption.
FHIR is an extensible standard that retains its core simplicity. At the same time, additional valid requirements that are not already part of the standard can be implemented as extensions. These extensions can be used to represent additional information that is not part of the resource's basic definition.
Other benefits of the FHIR standard include the following:
- All transactions are stateless since FHIR application programming interfaces (APIs) are aligned with the REST architectural style. This reduces memory usage and supports horizontal scalability.
- FHIR resources are suitable for exchange across the network.
- Highly optimized resource formats can be leveraged to improve performance in complex transactions across multiple connected systems.
- FHIR includes built-in mechanisms for clinical terminology linkage and validation.
- FHIR is easy to adopt and implement since it allows the use of industry standards and commonly known markup and data exchange technologies.
How FHIR works
The FHIR standard is built around two primary components: resources and APIs.
FHIR resources are basic units of exchangeable content that can be used to exchange and/or store data. The goal is to resolve clinical and administrative problems in healthcare. Both technical experts and nontechnical people can understand resources. Every FHIR resource has a known identity by which it can be addressed and contains a set of structured data items. Each resource also has an identified version that will change if its contents change. Also, a base language is defined for every resource, and all resources have a common set of metadata and a human-readable part.
FHIR information modeling uses a composition approach -- meaning that the base set of FHIR resources can be used by themselves or combined with other resources by using resource references. Such flexibility means that resources cover most common use cases, such as care plans and diagnostic reports. The standard's built-in extensibility can be leveraged to combine and tailor resources to cover other use cases.
When resources are exchanged, they can be represented in Extensible Markup Language (XML), JavaScript Object Notation (JSON) or Resource Description Framework (RDF Turtle) formats. In fact, FHIR resources are notionally equivalent to physical information models implemented in XML or JSON. The documents can be validated syntactically or against some predefined business rules to ensure high data fidelity and semantic interoperability.
The JSON and XML formats are similar in terms of object members, objects and arrays, and properties. However, there are differences as well. For example, there are no namespaces in the JSON representation and resource types are represented differently in JSON. Regardless of the format used, systems are required to declare which format(s) they support in their Capability Statement.
The Capability Statement describes the interfaces that an implementation exposes for data exchange. It is one of two special kinds of resources that are used in FHIR to describe how resources are defined and used. The other special FHIR resource is called StructureDefinition. It provides additional rules that constrain various aspects of the resources being used, including their data types and extensions.
FHIR is a RESTful specification, meaning transactions are performed directly on the server resource using an HTTP request/response mechanism. Also, FHIR supports Level 2 of the REST Maturity model. But again, extensions can be used to enable full conformance with Level 3 of the model. Health IT applications that conform to FHIR are specifically conformant to RESTful FHIR.
FHIR provides software development resources and tools for administrative concepts such as patients, providers, organizations and devices, as well as a variety of clinical concepts including problems, medications, diagnostics, care plans and financial issues, among others.
Unlike HL7's most widely used formal standard (also called HL7), FHIR is designed specifically for the web and provides resources and foundations based on XML, JSON, HTTP, AToM and Open Authorization (or OAuth) structures. Tools can be reused to improve interoperability to retrieve the history of a specific resource or a specific version. The specification is online, fully hyperlinked and can be linked from the resource of a property to the data type of that property. FHIR can be used in mobile phone applications, cloud communications, EHR-based data sharing and among institutional healthcare providers.
The FHIR specification is broken into three parts: general documentation, implementation and resource list. General documentation describes how resources are defined and gives background material including definitions of data types, codes and XML and JSON formats. Users can use resources with the RESTful API as clinical documents or in a service-based architecture.
FHIR defines a framework for extending and adapting resources, which can be read by any system, regardless of how they were developed. Extension definitions can be retrieved using the same framework as retrieving other resources. Each resource carries human-readable text representation using HTML.
The HL7 organization
HL7 is an international organization with members in more than 50 countries. Its leaders have complained that some bigger members, including vendors and healthcare providers, have failed to adequately support HL7's standards development work, particularly in regard to FHIR. The lack of funding has slowed the progress of FHIR, HL7 CEO Charles Jaffe, M.D., has alleged. Nevertheless, Jaffe and other HL7 leaders point out that FHIR is already being widely used by vendors and healthcare organizations to build and run health IT applications.
HL7 develops new standards using a multiyear balloting system in which members vote and add commentary in successive balloting rounds until negative comments are eliminated, draft standards, draft standards for trial use and formal standards are commonly agreed upon.
FHIR history
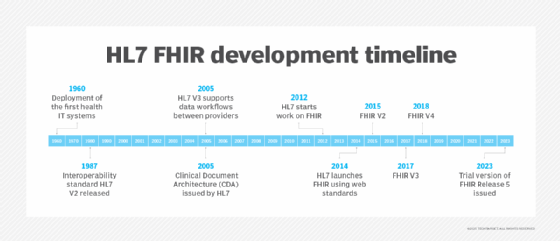
FHIR is a more recent standard compared to many other standards developed by HL7, including HL7 V2.x and CDA. Development on the FHIR began in 2012 as healthcare organizations and patients started calling for a standardized and easy way to access health data. At the same time, data volumes were growing, creating the need to share data in real time, ideally using globally accepted internet technologies and standards such as REST.
HL7 released the FHIR DSTU1 (First Draft Standard for Trial Use) in September 2014 and DSTU2 in October 2015. It wasn't until March 2017 that full FHIR Release 3 (STU - Standard for Trial Use) was published.
In 2018, HL7 released Release 4 (1st Normative Content + Trial Use Developments), followed by FHIR Release 5 (Trial Use), released in March 2023. This release is labeled "Trial Use" because the ballot cycle that led to it was performed under the HL7 Standard for Trial Use (STU). The content in this release is not considered normative, meaning it was not approved by the ANSI standards process in a previous version and is not considered to be stable. Also, changes may be made to the content in future versions.
Another significant FHIR effort, SMART on FHIR, is based at Boston Children's Hospital. It has also gained broad industry support. SMART on FHIR is a set of open specifications to integrate apps with EHRs, portals, health information exchanges and other health IT systems.
Additionally, HAPI FHIR is a complete FHIR implementation library in Java. HAPI, designed to be flexible and composable, was developed at Canada's University Health Network (UHN) with the goal of developing unified FHIR services for exposing data backed by different healthcare systems and repositories. Today, HAPI FHIR is open source and free to use. It is licensed under the Apache Software License 2.0.
Learn how a new HL7 FHIR accelerator aims to enhance medical device interoperability by creating FHIR implementation guides and supporting real-world testing.