What is telemedicine?
Telemedicine, also referred to as telehealth or e-medicine, is the remote delivery of healthcare services over the telecommunications infrastructure.
The principal goal of telemedicine is to provide a better experience for patients when dealing with healthcare providers. Telemedicine makes it possible for healthcare providers to evaluate, diagnose, communicate with and treat patients without the need for an in-person visit. Patients can communicate with physicians from their homes or offices using their own personal technology, such as a laptop or smartphone or by visiting a dedicated telemedicine kiosk.
How telemedicine works
A typical telehealth exam involves downloading an application or calling a telemedicine number, provided by a physician's office or a patient's employer as part of health insurance benefits. After sharing information about medical history and symptoms, the remotely located patient will be connected to a clinician or other qualified healthcare provider. Based on the medical professional's evaluation, the call typically ends with the patient receiving further instructions, including perhaps an over-the-counter or prescription medication to take, and a follow-up appointment, if needed.

Can patients trust telemedicine?
Trust plays an important role in the delivery of healthcare of all kinds. Patients need to trust that their doctors and other medical professionals have their best interests at heart. The need to feel confident that any medications being prescribed will be effective and not show any detrimental side effects. They need to trust their surgeons, anesthesia doctors and other attending personnel during surgical procedures.
This article is part of
AI in healthcare: A guide to improving patient care with AI
Telemedicine is one option for delivering healthcare. It is certainly not the only way to deliver patient care. Trusting telemedicine means trusting the technology connecting doctor and patient, that it will work when needed and not fail. Patients need to be confident that telemedicine costs can be covered by insurance. They need to trust that medical institutions, ranging from major hospitals to same-day clinics in drug stores, can support telemedicine and are committed to its effective use.
Technologies associated with the various forms of telemedicine are generally quite mature, as are the network services connecting doctor and patient. For patients with mobility challenges or in remote locations, telemedicine may be the best way to obtain the healthcare services they need. As such, they must be able to trust that telemedicine will be available when they need it, and that they can be connected to a provider -- even if it is not their primary care physician (PCP) -- who will provide the appropriate care they need, and ensure that other key players, such as their PCP, will receive the information needed to deliver the proper services.
Ideally, patients who use telemedicine as a primary means of obtaining healthcare should also have access to alternative ways to receive care, such as a family member or neighbor who can drive them to a medical facility. As such, patients should generally be able to trust telemedicine and, hopefully, depend on it without the fear of a bad experience.
Types of telemedicine
Telemedicine can be classified into four main categories that, in some cases, overlap.
- Interactive. Physicians and patients communicate in real time from a patient's home, office or a designated medical kiosk. They can interact using phones or video conferencing software that complies with Health Insurance Portability and Accountability Act (HIPAA) regulations.
- Remote patient monitoring (RPM). Telemonitoring-enabled RPM lets patients monitor their symptoms or condition from their home or office. They use mobile health devices, such as wearable technology (e.g., smart wristwatches), and applications that collect data about temperature, blood sugar levels, blood pressure and other vital signs.
- Store and forward. Also known as asynchronous telemedicine, this approach lets one healthcare provider share patient information, such as lab results, with another healthcare provider, assuming the patient grants permission to share that data.
- Mobile. Mobile telemedicine describes healthcare activities facilitated by mobile devices. These could include remote clinical services, such as consultations and patient-doctor communication through mobile patient portals, or public health activities, such as disseminating warnings about a dangerous outbreak.
Telemedicine is asynchronous and synchronous in how it works. Synchronous telemedicine occurs when a patient can connect in real time and one-on-one with a healthcare provider. This, for many patients, especially older adults, represents the ideal use of telemedicine by allowing patients to connect immediately with the doctor or other professionals. A subsequent in-person appointment may be needed and can be set up at the end of the call. Follow-ups to in-person or remote calls can also be conducted using telemedicine.
By contrast, asynchronous telemedicine makes a connection but not in real time. For example, prior to a doctor visit, an automated healthcare system requires that a patient answer a variety of health-related questions before checking in for the appointment. Calling into an automated system to order prescription refills is another example.
Preparing for a telemedicine appointment
Depending on the telemedicine technology being used, the level of interaction with the system before the actual call will vary. As noted, an asynchronous call may be needed to collect relevant patient data and the issues to be addressed. Data on healthcare insurance, family history, allergies, previous medical procedures, existing health conditions, recent travel within or outside the country, medications being used, and other information may need to be collected. The system will coordinate an appointment date and time, often on the same call. It may list the items needed for the call.
The synchronous part of the process occurs when the actual call takes place. At that time, the doctor and patient will go through an interview process, similar to an in-person visit. The doctor will recommend a treatment regimen, prescribe medications, and perhaps write up orders for medical tests or even surgical procedures. Once the issues have been addressed, doctor and patient agree on the next steps and proceed accordingly.
Pros and cons of telemedicine
Advancements in telemedicine have grown steadily over the past decades, making it a viable alternative to in-person healthcare visits. While the positive aspects are obvious -- convenience, timeliness -- a few downsides must also be noted.
The benefits of telemedicine for patients include:
- Convenience. Patients do not need to take time away from work or family for an appointment, and they save travel time and associated expenses, such as paying for gas and childcare. This can be useful for minor medical needs that do not require urgent care and for routine check-ins for patients with chronic conditions.
- Increased access. Telemedicine for patients in rural areas helps them obtain specialty health services, such as mental health treatment and post-surgery follow-up, that they otherwise might not get without traveling a long distance for an in-person visit.
- Reduced exposure. Telemedicine makes it possible for sick people to receive healthcare without the risk of infecting others or becoming infected themselves.
Telemedicine benefits healthcare providers in the following ways:
- Reduced cancellations and no-shows. With telemedicine, patients may be less likely to cancel or not show up for their appointments. Prior to the appointment time, a provider can remind the patient of the appointment and collect any pertinent data needed for the appointment.
- Encourage better choices. Telemedicine provides more ways for providers to communicate about and encourage a healthy lifestyle for their patients.
- More effective communication. Telemedicine encourages patients to engage more regularly with healthcare providers. This gives the provider a more accurate view of the patient, which can translate into a better foundation for treating them. For example, telemedicine consultations let the physician view the patient's environment in real time, which may provide additional insights for treatments.
- Patient education. Properly planned and delivered, patient education can be enhanced using telemedicine. Providers can deliver useful health information to patients, such as details on their treatment plan.
- Streamlined process. Depending on how the telemedicine communications resources are structured, telemedicine patients can be connected to the correct department or specialist and wait times reduced.
- Increased collaboration among departments. Telemedicine technology aids healthcare providers by allowing them to share patient information with other providers, which can provide better patient outcomes.
Some of the challenges associated with telemedicine include:
- Loss of connectivity. Disruptions to networks that support telemedicine, such as Wi-Fi and the internet, plus non-working smartphones or laptops, can make it difficult to communicate.
- Quality of service provided. Telemedicine users may not be connected directly with their primary healthcare provider and may have to deal with someone whose qualifications and experience are unknown.
- Loss or theft of patient information. Information communicated using telemedicine must be protected from unauthorized access and use, as must traditional electronic patient data.
- Costs. The costs associated with providing telemedicine must be considered, especially if healthcare insurance does not provide reimbursement.
Healthcare providers may be concerned with some of the potentially negative aspects of telemedicine, including:
- Security risks. Telemedicine systems depend on access to secure network infrastructures, and if that security fails, providers may be faced with data breaches. Healthcare organizations are among the biggest targets for online criminals and cybersecurity attacks.
- Regulatory complications. Differences among states regarding telemedicine legislation may complicate the delivery of healthcare services electronically. For example, states may require evidence of an established doctor-patient relationship before the doctor can issue a prescription.
- Technical challenges. Telemedicine health providers must be trained on how to use telemedicine equipment. Costs associated with deploying, managing and maintaining telemedicine technology may be steep. In addition to network costs, there may be costs for specialized equipment, such as integrated telehealth carts and encounter management software.
- Licensing issues. Certain states require providers who practice telemedicine across state lines to have a valid license in the state where the patient is located. This means providers may need to obtain and sustain multiple state licenses.
Financial considerations of telemedicine
For both patients and providers, telemedicine healthcare visits often are a less expensive way to provide medical care. Patients considering the use of telemedicine should check with their insurance provider to see if the services are covered.
Various payment models are used in telemedicine. Some health systems offer remote consultations as part of their regular care services; patients are charged based on insurance plans or government reimbursement schedules. A patient's employer may offer a virtual care option as part of health insurance coverage premiums. Patients without suitable insurance coverage may be able to use a telehealth vendor for a flat fee.
Telemedicine legislation in the U.S.
In recent years, many states have passed laws that make telemedicine easier to provide. Federal health regulators have explored ways to extend Medicare reimbursements for telemedicine services beyond December 2024, and they are currently set to expire September 30, 2025.
The Patient Protection and Affordable Care Act (PPACA) of 2010 has governed telemedicine in certain situations under Medicare, but telemedicine regulation for the most part falls to the states, with reimbursement delivered using Medicaid.
State-specific telemedicine legislation in the U.S. varies widely, especially related to these issues:
- Licensure requirements. Telemedicine providers must generally be licensed in the state where a patient is located. Collective arrangements for practicing across state lines have been established for both physicians and nurses.
- Temporary practice laws. Some states permit temporary telemedicine delivery for out-of-state providers under a variety of conditions.
- Telemedicine registration. Some states permit out-of-state providers to register for telemedicine services in lieu of obtaining a full license, assuming they meet specific criteria.
- Restrictions in some states. Telemedicine providers must carefully check the rules within states where they wish to practice, as prior telemedicine licensing waivers may have been eliminated.
- Data privacy regulations. While HIPAA typically governs healthcare IT activities, some states may have stricter rules on how telemedicine services are delivered and required data privacy practices.
What federal government agencies address telemedicine?
While the states are generally responsible for administering telemedicine rules and regulations, the following federal agencies also play a role in shaping telemedicine policies and programs in the U.S.
- Department of Health and Human Services (HHS). HHS oversees telemedicine and telehealth initiatives through subagencies, including:
- Centers for Medicare & Medicaid Services (CMS). CMS sets telemedicine policies for Medicare and Medicaid.
- Health Resources and Services Administration (HRSA). This agency addresses telemedicine in rural and underserved regions.
- Office for Civil Rights (OCR). OCR coordinates compliance with HIPAA regulations as applied to telemedicine.
- Drug Enforcement Administration (DEA). The DEA regulates how telemedicine is used when prescribing controlled substances
- Federal Communications Commission (FCC). Access to broadband network services for telemedicine is regulated by the FCC.
- Veterans Health Administration (VHA). Veteran access to telemedicine resources is facilitated by the VHA.
- Centers for Disease Control and Prevention (CDC). Public health initiates using telemedicine are supported by the CDC.
History of telehealth
The development of modern telemedicine and telehealth began with development of telecommunication technology and its associated infrastructure, particularly the telephone and telegraph. In the early 1900s, for example, heart rhythms were transmitted over the telephone in the Netherlands. Telemedicine technology was used in military situations during the Civil War when telegraph messages were used to order medical supplies and report casualty and injury lists.
The first transfer of a medical image occurred in 1948 in Pennsylvania, when radiology images were sent over a telephone line. Canadian radiologists created a similar teleradiology system for use in Montreal. In 1959, clinicians at the University of Nebraska transmitted neurological examinations across campus to medical students using two-way interactive television.
Early computer-based patient records were in use in the 1960s. Electronic medical records (EMR), also called electronic healthcare records (EHR), started to be more widely used in the 1980s. As part of the American Recovery and Reinvestment Act, healthcare providers were required to show "meaningful use" of EMRs by January 1, 2014, to maintain their Medicare and Medicaid reimbursement levels.
In the early days of telemedicine, healthcare professionals used the technology to reach patients living in rural and underserved areas. This is still important today, and the technology continues to expand into urban areas, especially those with healthcare shortages.
Today, telemedicine is used in these applications:
- Hybrid care models that combine in-person and virtual delivery
- Advanced electronic devices and medical systems using artificial intelligence (AI)
- Development of hospital-at-home programs
- Behavioral health and psychiatry
- Complex medical cases and procedures
How will AI impacts telemedicine?
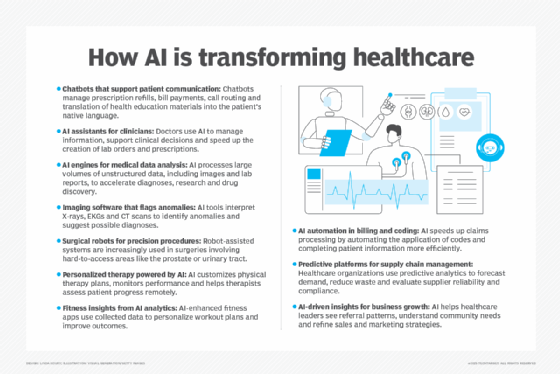
AI and the Internet of Things (IoT) have been supporting the advancement of telemedicine by enhancing these healthcare activities:
- Better diagnostics. AI can assimilate a large amount of patient data and deliver a broad range of analytics, diagnostics and treatments.
- Individual care. Activities such as treatment plans designed for individual patients based on their data are expected to improve outcomes and patient satisfaction.
- Remote healthcare monitoring. Remote capture and analysis of patient data can help detect early signs of health issues and facilitate timely interventions.
- Workflow Optimization. AI can automate many repetitive processes such as scheduling and documentation, which provides more time for patient care.
- Remote virtual assistance. An example of asynchronous telemedicine is where AI-based chatbots and virtual assistants deliver patient support, such as answering questions, scheduling appointments, updating patient data and providing guidance on healthcare strategies.
What is the future of telemedicine?
Assuming that regulators, government agencies, healthcare organizations and insurers and medical professionals continue to use telemedicine, the future is indeed very bright. Among the trends and developments shaping its future are:
- Expanded use of AI. As noted, artificial intelligence and IOT are likely to be significant components of telemedicine systems.
- Remote monitoring. Wearable devices such as smart watches and home-based medical systems help medical professional by monitoring their patients and the status of their health.
- Greater reach. As networking resources expand into rural and underserved areas, telemedicine availability and use will increase.
- Tech advances. Continued development of technologies such as 5G mobile service, augmented reality (AR) and virtual reality (VR) will greatly enhance real-time patient-doctor interactions.
- Emphasis on preventive care. AI and other technologies will deliver better patient analytics and preventive healthcare, often by identifying issues before they become serious.
- Collaboration globally. Information and expertise sharing using telemedicine can reach globally, making critical information available to healthcare entities everywhere.
- Telemedicine regulations and legislation. Periodic reviews and updates to laws and regulations governing telemedicine should increase its use.
Telemedicine use will continue to expand through advances in technology, development of new applications and a greater focus on preventive healthcare to elevate the delivery of healthcare. As telemedicine use advances, there will be a need for ongoing regulatory oversight and reform to ensure patients are protected.
AI is transforming telehealth by improving triaging, image analysis, patient diagnosis, treatment planning, monitoring, and mental health support. Learn more about how AI is changing telemedicine.






