AI in healthcare: A guide to improving patient care with AI
AI is permeating critical healthcare practices, from interpreting mammograms to discovering life-saving drugs, while surgically transforming hospital workflows.
AI's potential to revolutionize the way organizations conduct business has been scrutinized for decades, and even more so since generative AI came into focus less than three years ago. While AI hyperbole has outweighed reality in many industries, the healthcare sector is a notable exception. AI technologies are playing a critical role across medical services -- from diagnosis and personalized care to records management and billing.
AI’s ability to ingest and process vast volumes of data with startling speed has proved widely applicable in a field where time-sensitive decisions are made based on medical images, test results, patient medical records and other life-impacting data. AI's predictive capabilities not only help diagnose illnesses and diseases, but they also predict potential drug interactions, recommend patient treatments, arrange ongoing care, and improve patient outcomes. In addition, AI plays an increasing role in patient management, drug discovery and development, and administrative processes.
For these reasons and more, the healthcare industry's appetite for AI investments is expected to grow at an astonishing rate -- 38.6% annually over the next five years, driven by deep learning, care for seniors and chronic care management, according to research firm MarketsandMarkets. Likewise, McKinsey & Company cites multiple catalysts for healthcare's surge in AI investments, including generative AI (GenAI), back-office use cases, claims processing and insurance verification.
"AI is turning healthcare on its head as we know it," said Shannon Germain Farraher, senior analyst for healthcare at Forrester. Healthcare organizations still struggle with a host of endemic issues, Germain added, pointing to labor shortages, tight budgets, administrative burden, the volatility in today's regulatory restructuring, as well as taxing relationships among payers, providers and pharma. "Many see AI as an answer to these issues," she said, "while others see a future where they need to have AI just to stay competitive and relevant, never mind operationally and financially efficient."
This comprehensive guide examines many aspects of AI in healthcare, including applications, benefits, challenges, technologies and trends. Readers will also get a big-picture analysis of what healthcare and health IT professionals must do to successfully implement AI while addressing critical ethical and compliance issues. Hyperlinks, research and comments presented throughout this page connect to related articles that provide additional insights, new developments and advice from healthcare industry experts.
How AI is reshaping applications in healthcare today
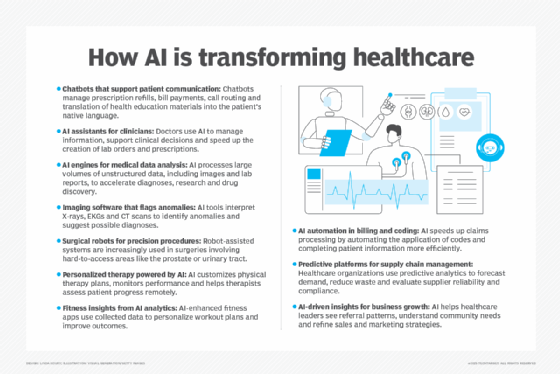
AI's multitude of capabilities is reshaping the everyday clinical and administrative workflows of hospitals, health systems and large medical practices. Depending on the application, healthcare organizations can implement AI tools through pilot programs, individual service lines, or patient populations. They can also augment AI-enabled processes, such as the electronic health record (EHR) system, with additional AI capabilities. Several healthcare practices, including the following, are heavily influenced by AI.
Patient engagement. AI-based chatbots in healthcare facilitate patient interactions such as scheduling an appointment, refilling a prescription or paying a bill. Depending on the degree of difficulty, chatbots can determine whether a patient needs to speak to a person based on medical symptoms or the complexity of the patient's needs. Chatbots can also provide evidence-based recommendations or translate educational resources into a patient's native language.
Clerical support for physicians. AI can be used to document patient visits, draft post-visit notes to patients, manage information and support clinical decisions. Relieved of the burden and stress of paperwork, physicians can spend more of their time interacting with patients. AI systems enabled with ambient clinical intelligence are used in examination rooms to retrieve information from the EHR system as well as capture notes and create instructions for prescriptions or lab orders.
Documentation. GenAI in healthcare is focused on administrative use cases that improve the quality, speed and efficiency of healthcare documentation, according to a February 2025 survey published by the American Medical Association. GenAI models can process enormous amounts of medical data from EHRs to identify missing information. Microsoft reported its augmented AI assistant saves clinicians about five minutes per patient encounter, while Oracle announced its clinical AI agent reduces documentation time by nearly 30%.
Data analysis. Most healthcare data, including medical images and lab reports, is unstructured. AI systems can parse unstructured data sources much faster than traditional analytics tools. Depending on the algorithm, AI models can provide diagnostic insights, identify high-risk patients, recommend treatments or help hospitals prevent harmful drug interactions.
Imaging interpretation. Human analysis with the naked eye can be time-consuming and prone to error. Image recognition tools can interpret studies such as X-rays, electrocardiograms and CAT scans to identify irregularities, make a computer-aided diagnosis or deliver normal results so radiologists can focus on more complicated studies.
Robot-assisted surgery. Though used for decades, robot-assisted surgery is now aiding surgeons during procedures involving tight, cramped and sometimes inaccessible areas like the prostate and urinary tract. This minimally invasive approach can speed up recovery times and reduce hospital stays. Robotic systems might also perform minor tasks, such as suturing, in the future.
Drug discovery and development. The drug development lifecycle takes billions of dollars and decades of research, with no guarantee of regulatory approval from the U.S. Food and Drug Administration. Integrating AI technologies into drug discovery, development and manufacturing processes can help pharmaceutical companies get new drugs to market faster and more efficiently. AI and machine learning tools are improving process optimization, predictive maintenance and quality control, while flagging data patterns a human might miss.
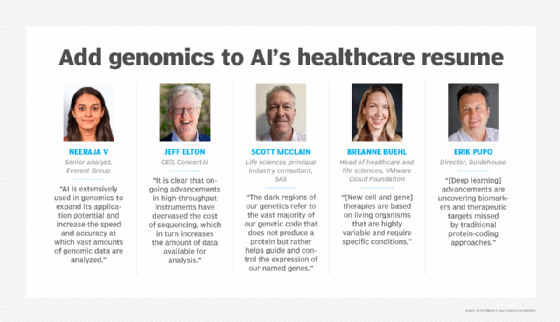
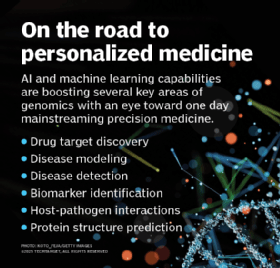
Genomics research. Recent AI advancements in computing, management techniques, algorithms and multimodal large language models are boosting genomics research. AI is also improving the speed and accuracy of drug target discovery, disease modeling and detection, and gene therapy, aiding clinicians in delivering personalized, precise medical treatments to patients.
Telemedicine. AI supports remote healthcare services delivered over telecommunications infrastructure. Telehealth use cases include medical image analysis, virtual triaging of patients, virtual care assistants, chronic disease management, mental health check-ins, patient monitoring in clinical settings, as well as contact center, administrative and clinical assistance.
Remote patient monitoring. AI can be incorporated into remote patient monitoring tools or used to streamline RPM data processing to provide patients with care outside a hospital environment. AI bolsters biosensors and wearables to help care teams gain insights into a patient's vital signs or activity levels, predict clinical complications and identify patients likely to benefit more from hospital-at-home services than inpatient care.
Physical therapy. It can be difficult for physical therapists located at a single site to provide consistent treatment for patients across different locations. Therapists can use AI to analyze patient data and provide personalized treatment recommendations to each patient. By incorporating virtual reality into physical therapy treatments, patients can receive immediate feedback on their training regimen while clinicians monitor the patient's progress.
Revenue cycle management. Before AI and automation, insurance claims processing was mostly manual and frustrating for patients forced to spend long periods of time on the phone. Automation speeds up various stages of the RCM process, such as applying the right medical codes to a patient visit or filling in demographic information.
Supply chains. Managing the proper inventory, cold storage requirements, and expiration dates for vaccines, medications and other supplies is tricky business. Predictive analytics improves inventory management by tracking historical data, anticipating demand and monitoring shipping deadlines as well as product safety requirements.
Business strategy. Hospitals and health systems can find themselves in highly competitive markets when it comes to adding and retaining patients. Sales and marketing teams can use AI to provide analysis and insights into patient populations that will help businesses make more informed decisions that drive revenue growth.
Ethics: How AI can be thoughtfully implemented in healthcare
While there have been significant tangible benefits of AI in several key areas of healthcare, the race to achieve positive outcomes and medical breakthroughs can conflict with the ethical administration of patient medical treatments.
The healthcare industry is ethically responsible for ensuring sensitive patient data is protected in accordance with prevailing regulatory obligations, such as patient data privacy standards. It's also responsible for ensuring that patient data is used appropriately so that healthcare providers and AI systems "do no harm" -- a fundamental principle of the Hippocratic Oath. It's also responsible for ensuring patient information is used in a transparent and responsible manner to mitigate decision-making bias while guaranteeing patient anonymity.
AI is far from perfect, so when AI is used in healthcare, providers are duty-bound to ensure it doesn't violate their own standards. Ethical application of AI in healthcare entails three basic considerations:
- Accuracy. AI assistance in healthcare should never be taken at face value. While the information AI provides can save lives, its conclusions should always be examined and validated by human experts.
- Fairness. AI outcomes are only as good as the underlying data. Incomplete, inaccurate and biased data can lower the accuracy of its conclusions and negatively affect healthcare decision-making.
- Security. Safeguarding sensitive patient data from illegitimate or inappropriate access requires extensive security to ensure data used to train AI systems is anonymized properly, so conditions and outcomes can't be traced to specific patients. AI security requires a holistic approach that embraces commitments from IT and healthcare professionals.
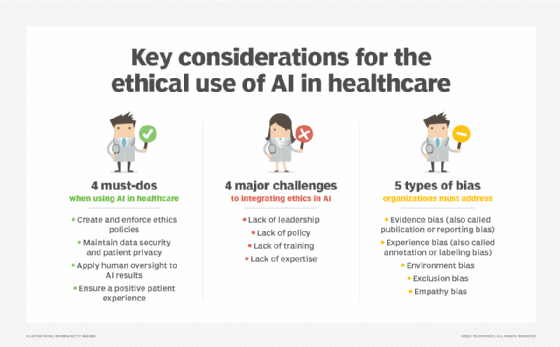
Developing and adhering to ethical standards and policies can be daunting for AI-driven healthcare organizations. Problems can ensue due to a lack of leadership, policies, training and expertise. The following best practices can ensure these organizations use AI tools, technologies and techniques wisely and for the benefit of patients, while protecting themselves against ethics violations:
- Executive support. The ethical use of AI must start at the top of the healthcare organization, with senior leadership recognizing the need for adherence to ethical standards and issuing a mandate for the ethical use of AI systems. This entails understanding the risks of AI related to data protection, data ownership, data quality, data bias, informed patient consent, accountability and liability.
- Comprehensive AI policies. Detailed policy frameworks help guide the use of AI systems, translating AI recommendations into clinical practice and ensuring AI transparency and explainability. Policies include information on patient consent and equal access to care, ensuring AI doesn't dehumanize patients, and addressing AI errors, AI bias and outright AI system misuse.
- Mandatory training programs. Governance policies around ethical AI use must be communicated and reinforced across the entire healthcare organization by making meaningful AI ethics training mandatory for all clinical and administrative staff.
- Adherence to privacy regulations. Adhering to the strong regulatory and legislative statutes already in place to safeguard patients' personally identifiable information addresses many ethical issues related to AI use. The following practices are required: getting patient consent on how data is collected and used, collecting minimal data, following data storage and security protocols, using identity and access management tools, and implementing data backup and disaster recovery measures.
- Human oversight of AI at several levels. AI recommendations should always be reviewed for accuracy; AI-based health decisions need to be explainable and checked to account for subjective uses, such as patient preferences and values. Liability and other legal issues that affect the entire AI system chain must be considered, along with regular training in the proper and acceptable use of AI tools.
- AI experts on staff. Extensive knowledge of AI systems and detailed insight into the organization's computing infrastructure are paramount and demand an expert staff that understands and supports ethical integration efforts with AI systems. A gap in expertise can compromise AI ethics initiatives and put the healthcare organization at risk.
- Patient-centric focus. Patient treatment at several levels includes empathy and sensitivity in information-gathering, recognizing and respecting patient preferences and values, and following up on patient outcomes as well as the quality of care. Clear and concise patient consent should explain the information collected, why it's needed and how it's used, with the option for patients to opt out of certain data uses.
What benefits come with using AI in healthcare?
AI has the potential to help healthcare organizations cut costs, improve patient care and relieve providers of manual tasks, such as documenting patient visits. Healthcare was among the first industries to put AI to work in a practical way. From operating rooms to research laboratories to billing departments, AI is becoming widely integrated into the workflows of healthcare organizations. GenAI appears to be the most recent catalyst. The accessibility of GenAI models, Forrester's Germain noted, has contributed to patient and healthcare employee adoption of AI-assisted services.
A majority of healthcare systems use AI, according to the "AI Adoption and Healthcare Report 2024" released late last year by the Healthcare Information and Management Systems Society (HIMSS) in partnership with Medscape. The HIMSS survey of IT and medical professionals found that 86% of hospitals and health systems use AI and that 43% had been using the technology for at least one year -- a significant increase from just 19% of hospitals reported in a 2022 American Hospital Association survey.
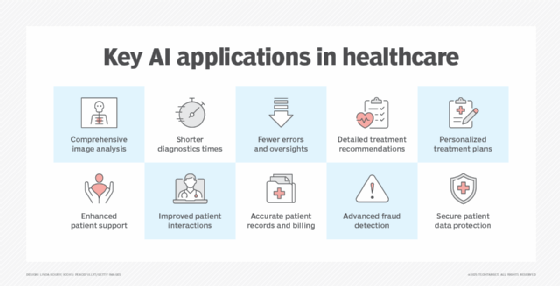
AI systems benefit several areas of healthcare, including diagnostics, patient treatments, administration and patient experience. AI's ability to ingest and analyze massive volumes of raw and unstructured data, from medical images and blood work to emergent data -- i.e., data inferred from non-healthcare records like social media and search queries -- means that healthcare providers can be alerted to a potential disease or illness far earlier than by direct human examination. By shortening diagnostic times, patient treatments can be faster, less intrusive and less expensive. AI can also double-check human diagnoses and cross-check treatments or medications against available digital health records and patient profiles, potentially reducing diagnostic errors, avoiding unnecessary or ineffective treatments and preventing dangerous drug interactions.
AI used in genomics to provide speed and accuracy in drug target discovery, disease modeling, disease detection and gene therapy holds promise for mainstreaming personalized and precise medicine in the future. AI genomics tools could be combined to potentially make genomics data more accessible, enhance various aspects of health research and open new opportunities for discovery in many key health science-related areas, including dark DNA, spatial biology, gene editing and omics, which entails the various disciplines of biology relating to genomics.
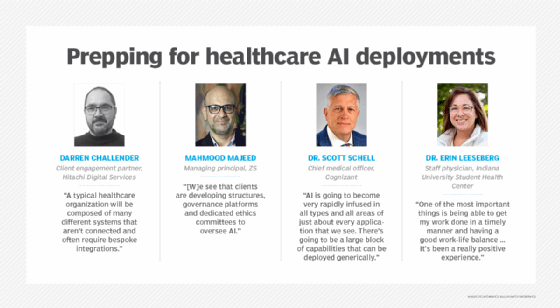
Healthcare providers and office staff are often so overwhelmed with burdensome paperwork that patient interactions can suffer, making health services frustrating and disappointing for many patients. Using AI in clinical documentation, for example, has helped Dr. Erin Leeseberg, a staff physician at Indiana University's Student Health Center, work more efficiently on behalf of her patients. She noted that her use of Sunoh.ai's product has reduced her clinical note-taking chores by 5 to 15 minutes per patient. "One of the most important things is being able to get my work done in a timely manner and having a good work-life balance," she said. "It's been a really positive experience."
AI capabilities can also improve several aspects of healthcare administration, including the following:
- Enhanced scheduling capabilities, using natural language chatbots to make, change or cancel appointments and answer basic medical questions.
- Interactive assistance with medical billing issues, including patient financial obligations like copays and financing costs not covered by health insurance.
- More accurate billing and faster, more comprehensive patient record management by tracking medical procedures and applying proper coding.
- Predictive analysis for patient visits, records, care and billing to uncover potential healthcare fraud or illegitimate activity.
- Oversight to ensure only authorized users can access patient data and that any uses of the data are conducted securely, ethically and in compliance with regulatory obligations.
What challenges are associated with using AI in healthcare?
Poorly managed AI deployments could result in several dangerous side effects, including biased data, security breaches, patient privacy violations and disrupted staff-patient communications. And ill-conceived and hastily executed projects are unlikely to generate ROI.
To realize the full benefits of AI in healthcare, there are several hurdles healthcare organizations must overcome as they cope with the ethical use of data, regulatory obligations like HIPAA, safeguarding protected health information and potential liability issues.
Understanding AI
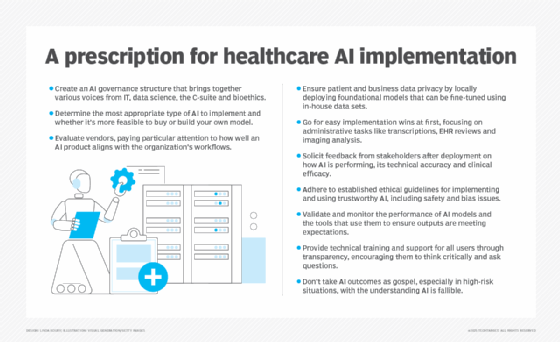
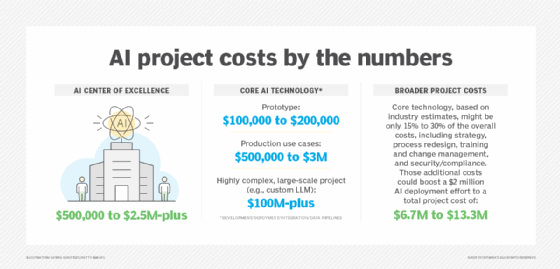
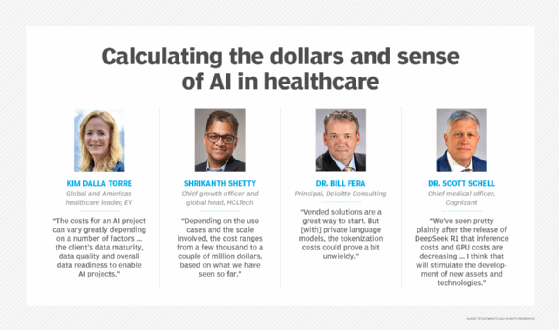
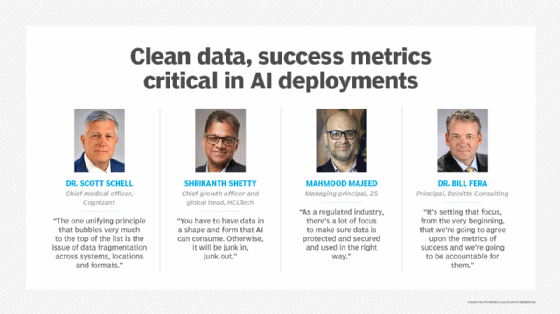
The foremost obstacle for healthcare organizations considering AI adoption is grasping the essentials of the technology and developing an AI strategy and vision. The two main objectives of an AI strategy should be to make business operations more efficient and develop new sources of revenue. Given the cost of a typical AI project, it's best to select an AI deployment with the greatest ROI potential. But a major sticking point is defining the parameters for success and measuring ROI.
"Historically, organizations have not been great about measuring success from the beginning, baselining and tracking to make sure that the hypothesis behind the deployment of the AI or GenAI tool is actually realizing the value we anticipated," Deloitte consultant Dr. Bill Fera acknowledged. An AI governance structure of relevant stakeholders, including clinicians, business leaders and finance executives, can help healthcare organizations identify use cases, deploy projects and track their progress. That structure, however, shouldn't come at the cost of stifling innovation.
Obtaining quality data
Another ongoing challenge is data -- and the fragmentation of it in most organizations. Fragmentation makes data difficult to use in AI models and can lead to poor outcomes. Providers, payers, pharmacies and testing laboratories use a multitude of standards to house data, forcing healthcare organizations to expend enormous effort gathering, cleaning and harmonizing their data so it's reliable and AI can make sense of it.
Data fairness, privacy and security
Ethical AI use aims to ensure healthcare AI models don't reflect bias that could skew data to the detriment of racial or ethnic groups. In addition to ethical considerations, healthcare organizations must factor regulatory compliance into their AI projects. The security and privacy of AI models call for appropriate boundaries. Security and patient data privacy should be integrated into AI systems during -- not after -- the time they're built.
Another data privacy issue is "bring your own AI" (BYOAI), when employees use their own AI tools, such as chatbot interfaces, for various tasks that involve sensitive information, instead of relying solely on AI tools provided or approved by IT. "BYOAI," Germain warned, "has to be managed closely and dealt with because of the ethical, responsible and safety implications, especially in healthcare."
Change management
New ways of doing business come with fears of obsolescent skills and vastly changed -- or eliminated -- roles, so employee training and change management are key, including AI literacy programs, hands-on training and industry certification. Organizations must consider the effects of AI on patients and their families as well as on healthcare workers. Patient outcomes could be compromised if AI disrupts the daily interactions among the parties.
Monitoring AI performance
Smaller healthcare practices might be at a disadvantage compared with large hospitals and health systems. Community-based, rural or federally qualified health centers often lack strong AI governance or the expertise to monitor AI system performance.
Providers, payers and life science entities can overcome the challenges of AI integration by focusing on ethics, security, data quality and user adoption to keep initiatives on track, along with a strategy that incorporates clearly stated goals and reliable methods to track progress.
What will the modern healthcare system look like in the future?
The Mayo Clinic has a wish list for the future of AI in healthcare, which it calls a "data-driven healthcare revolution." The list includes selecting and matching patients with the most promising clinical trials, developing and setting up remote health-monitoring devices, detecting currently imperceptible conditions and determining disease-risk years in advance.
"In the future, all healthcare organizations will be intelligent entities," Germain conjectured. "Becoming an intelligent healthcare organization requires optimizing workflows and elevating employee and customer experiences." Germaine pointed to six hallmarks that will characterize future healthcare systems, including smart hospitals: connected and validated clinical workflows, superior employee experiences, personalized healthcare, consumer-owned data, automated clinical safety interventions, and digital identities as well as verifiable credentials.
Other AI-enabled improvements on the horizon include the following:
- Using an array of nuanced data collected from patients to identify the onset of rare diseases, leading to faster and more effective interventions.
- Predicting the rate and implications of disease progression, leading to more timely and effective treatments while mitigating potential complications.
- Processing data from medical sensors and interpreting images in video feeds from exam rooms and surgical facilities, providing detailed assessments and procedural recommendations to practitioners in remote locations or places where human clinicians are limited in number and expertise.
- Interpreting a patient's genetic and genomics data to provide detailed treatment plans specific to the patient under the umbrella of precision medicine, including creating and manufacturing drugs crafted for the individual. Developments might include multimodal data integration, real-time analysis, standardized biobanks and more clearly defined regulations for AI use.
- Increasing the presence of agentic AI in healthcare to help with administrative tasks, call up insurers to seek pre-authorization for a treatment, write drafts of notes, provide summaries of patient encounters, check in with patients daily and collect patient data points that can be fed into a predictive model.
Ron Karjian is an industry editor and writer at Informa TechTarget covering business analytics, artificial intelligence, data management, security and enterprise applications.
John Moore is a writer for Informa TechTarget covering the CIO role, economic trends and the IT services industry.
Stephen J. Bigelow, senior technology editor at Informa TechTarget, has more than 30 years of technical writing experience in the PC and technology industry.






