What is ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification)?
The International Classification of Diseases, Ninth Revision, Clinical Modification, also known simply as ICD-9-CM, was the U.S. healthcare system's adaptation of the World Health Organization's (WHO) ICD-9 standard list of alphanumeric codes to describe medical diagnoses and procedures and to track diseases and mortality. Standardizing these codes helps to bring greater consistency among U.S. medical professionals in recording patient symptoms and diagnoses, especially for the purposes of medical billing and coding, payer claims reimbursement and clinical research. It also helps with the documentation and classification of morbidity and mortality data.
The U.S. Department of Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS) created ICD-9-CM as an extension of the WHO's Ninth Revision, International Classification of Diseases (ICD-9). The WHO established the ICD in 1948 and then expanded it over the years to track mortality statistics across the world. Simply put, ICD was a classification and reporting system for the causes of morbidity and mortality.
Since its early days, the system has been regularly updated to include new diagnoses, tests and procedures. The ICD-9 was ratified in 1975 at a WHO conference and published in 1977 by the WHO's Department of Knowledge Management and Sharing. Its four-digit-level categories and optional five-digit subdivisions helped to bring greater granularity in documenting and reporting diagnoses and procedures, as well as morbidity and mortality statistics.
The United States adopted the system in 1979 as ICD-9-CM to allow for the standardized capture of enhanced morbidity data and to enable diagnostic coding in inpatient, outpatient and surgical/procedural settings. It was succeeded by ICD-10-CM and ICD-10-PCS, used for diagnostic and procedural medical coding, respectively. The Protecting Access to Medicare Act of 2014 mandated all parties covered by the Health Insurance Portability and Accountability Act (HIPAA) implement ICD-10-CM and ICD-10-PCS by Oct. 1, 2015.
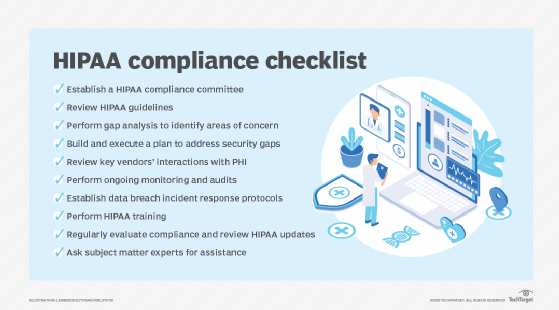
More broadly, the ICD system remains the lingua franca upon which most of the U.S. healthcare payments system is based. In addition to billing, the ICD system is also used for many clinical and healthcare applications for reporting and morbidity statistics. It is one of several code sets used under HIPAA for medical diagnoses, procedures, testing, treatments and supplies. Other notable code sets outlined in HIPAA include the Health Care Common Procedure Coding System, Current Procedure Terminology, Code on Dental Procedures and Nomenclature and National Drug Codes.
ICD-9-CM code structure
The ICD-9-CM system consists of three components:
- A numerical list of disease code numbers.
- An alphabetical index to every disease entry.
- An alphabetic index and tabular list of medical procedures (surgical, diagnostic, therapeutic).
The ICD-9-CM code set was updated annually, ultimately amounting to nearly 18,000 codes by the time of its retirement in 2015. It comprised three volumes -- until ICD-5, the entire system was contained in a single volume -- with each entry corresponding to a diagnosis or procedure. The codes refer to tabular lists of diseases, procedures and supplementary classifications, each following a standard format. Volumes 1 and 2 of the ICD-9-CM pertained to diagnostic codes, with volume 1 containing a numeric listing of diseases and volume 2 used by healthcare providers and facilities to locate the codes in volume 1. Volume 3 contained procedural codes (table plus index) used by hospitals to report services.
The ICD-9-CM codes could be entered onto a patient's electronic health record (EHR) and used for diagnostic, billing and reporting purposes. Related information also classified and codified in the system included symptoms, patient complaints, causes of injury and mental health disorders.
In the United States, changes and modifications to ICD codes are managed by the Centers for Disease Control and Prevention, the National Center for Health Statistics (NCHS) and CMS. There are four organizations identified as "Cooperating Parties" for the ICD-9-CM: the NCHS, CMS, American Hospital Association and American Health Information Management Association. The same four entities are Cooperating Parties for ICD-10-CM and ICD-10-PCS.
ICD-9-CM vs. ICD-10-CM
In the U.S., the passage of HIPAA made it mandatory for health plans, healthcare clearinghouses and the medical coders and billers who work for them, as well as healthcare providers transmitting any electronic health information, to adopt ICD-9-CM. The diagnostic codes in volumes 1 and 2 were adopted under HIPAA for all healthcare settings, while the procedure codes in volume 3 were adopted for all hospital-reported inpatient procedures.
Following the WHO's endorsement of ICD-10 in 1990, the first WHO member states adopted it four years later. The tenth edition greatly expanded the number of codes, today amounting to approximately 155,000. Notably, in its U.S. implementation, it was separated into two code sets: ICD-10-CM for diagnoses and ICD-10-PCS for inpatient procedures. This expansion provided considerably more specificity in identifying diseases, conditions and other data covered by the system. Its updated format -- increasing the maximum number of characters from five to seven -- also built in more flexibility for future expansion.
After several delays, U.S. law required all entities covered by HIPAA to transition to the new set of codes for electronic healthcare transactions included in the tenth edition by Oct. 1, 2015.
To a large extent, the implementation timing for ICD-10-CM coincided with other major U.S. health IT initiatives, including nationwide EHR adoption, establishing national health information exchanges and data-intensive accountable care organizations.
Prior to the congressional mandate, the tenth edition faced pushback from some physicians and hospitals that cited it as too cumbersome in terms of clinical documentation and overly complicated for common patient care episodes. Also, transitioning from ICD-9 to ICD-10 required significant workflow changes in clinical practices to ensure full reimbursement.
In 2022, the World Health Assembly adopted the next version of the International Classification of Diseases with ICD-11, further simplifying coding and expanding the scope with a whole host of improvements. Entirely digital, ICD-11 is designed to be more usable in IT environments. It is currently unclear when and how the U.S. will adopt ICD-11.
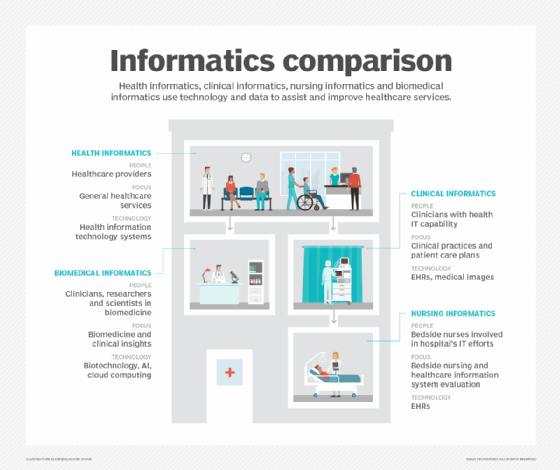
Learn the four levels of health data interoperability outlined by the Healthcare Information and Management Systems Society and see why medical specialty societies are key to advancing health data standards. Explore what role EHRs play in clinical informatics and how health information exchanges can support public health and equity.